Medicaid Unwinding: Resources to Keep Minnesotans Covered
375,000 Minnesotans are at risk of losing health coverage as eligibility reviews return for the state’s public programs, Medical Assistance and MinnesotaCare
Last month, Minnesota officially began the process of “unwinding” the COVID-19 pandemic-era policy that paused eligibility reviews for those on the state’s public health care programs, Medical Assistance (Minnesota’s Medicaid program) and MinnesotaCare.
These programs are critically important and currently provide health care coverage for 1 in 4 or 1.5 million Minnesotans. State programs cover 4 in 10 children, 4 in 10 births, 1 in 3 people with disabilities, approximately half of nursing home costs and about half of substance-use-disorder treatment. They also cover a disproportionate number of Black, Indigenous, and other People of Color in the state, highlighting potential health equity impacts for changes in these programs.
As eligibility reviews resume for the state’s public programs, Council members are working diligently to help Minnesotans maintain their coverage or successfully transition to new coverage.
The stakes are high. An estimated 375,000 Minnesotans could potentially move off public coverage during this process. Health care coverage provides many benefits, including helping pay the high costs of medical care and medications, coordinating services, connecting people to social supports and helping people access preventive care. Disruptions in coverage can have a serious negative impact and worsen health outcomes as well as create financial burdens and barriers to accessing timely and needed care. Early data from 20 states that have already resumed renewals show that over a million enrollees have lost coverage during this process between April 1 and June 12. There are wide variations between states in both renewal rates and the share of procedural disenrollments – where people lose coverage because they did not complete the enrollment process but may still be eligible for Medicaid.
These numbers highlight the challenges to make sure Minnesotans most at risk for losing coverage have access to necessary information and resources to maintain coverage during this process. With estimates that nearly half of those losing coverage will likely be due to procedural issues, like incomplete or missing paperwork, public awareness is a serious concern. Data from a recent survey found that nearly two-thirds of Medicaid enrollees were not aware that states are now permitted to resume disenrolling people from Medicaid programs, underscoring the need to increase outreach on this topic and help people learn how to successfully renew their coverage or transition quickly and seamlessly to other coverage.
Confronting the state’s unique challenges to keep Minnesotans covered
In Minnesota, renewals must be completed on paper and all renewal forms and important information will be sent via the mail. Because DHS had not collected eligibility information since the beginning of the COVID-19 public health emergency, many people are at risk of procedural disenrollment if their contact information is no longer correct.
Nearly half of Medicaid enrollees have not been through the renewal process before and certain populations are especially at risk of losing coverage – particularly children, people without stable housing, non-native English speakers, people living in high social vulnerability index (SVI) neighborhoods, and people with complex conditions. Due to the disproportionate share of BIPOC Minnesotans on the state’s public health care programs, a higher burden of coverage loss will also fall on these communities.
National studies show that 30% of people don’t know where they’ll find other coverage if they are no longer eligible. And an analysis of the impact of the expiration of the public health emergency estimates the uninsurance rate in Minnesota – which is now at a historic low of 4% – could increase significantly.
Support from the state’s nonprofit health plans for Minnesotans during the Medicaid Unwinding period
Council members have been working closely with many partners to raise awareness and share resources and best practices to ensure no one faces an avoidable gap in coverage. For example:
- Health plans are using care coordinators and other staff to assist members with questions and help complete their renewals
- Health plans are using data from DHS on renewal dates or coverage changes to reach out and help their members maintain their coverage
- Health plans are participating in the DHS Equity Partnership to ensure no Minnesotans fall through the cracks
The Council developed the following resources (also available on the Medicaid Unwinding Resource Page) for various stakeholders to raise awareness and support Minnesotans in maintaining health care coverage:
Enrollees-
- Fact Sheet with Enrollee Resources to Prevent a Gap in Coverage, with key steps:
- Update your contact information with your county, tribe, or health plan.
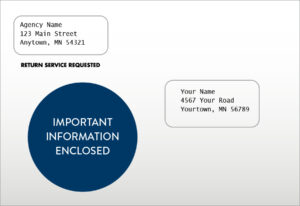
- Watch for the circle in blue when it’s time to renew. Important information will come in the mail in an envelope like this:
- Information on how to complete a renewal is available at https://mn.gov/dhs/renewmycoverage/
Employers-
- Fact Sheet with Employer Resources to Support Employees Transitioning to ESI
- “Have an Employee Who’s Losing Medicaid Coverage?” Fact Sheet (English)
- “Have an Employee Who’s Losing Medicaid Coverage?” Fact Sheet (Spanish)
Health Care Providers-
- Fact Sheet with Provider Resources to Help Patients Prevent a Gap in Coverage
Community Partners-
- Fact Sheet with Community Resources to Keep Minnesotans Covered
During the COVID-19 pandemic, the state’s nonprofit health plans played a leading role in safeguarding the health of Minnesotans providing over $2.6 billion in COVID-related medical costs, keeping people connected to care, and taking a nimble and innovative approach to support members throughout the state during a time of great need. As the nation and state move on to this next chapter of pandemic recovery, it is important to understand the significant implications of the Medicaid unwinding process and how we can all work together to make sure that Minnesotans stay covered and continue to have access to affordable and timely care.

