Prescription Drugs: Fact Check
Even those of us who don’t take any prescription drugs, pay for the high prices because they are included in the health insurance premiums we pay every month. Today in Minnesota, $1 out of every $5 in medical bills is for prescription drugs we get at our clinics and local pharmacies. There’s a lot happening today with prescription drugs and there is more news on the way.
Why are drugs so expensive?
Who oversees drug prices?
Drug companies set the prices. Unlike insurance or many other public services, no agency or regulator reviews drug company pricing. In the past few years, the prices have been set so high that a $65,000 price is hailed as a success.
How much does it cost to develop a new drug?
Depending on who you listen to, it costs on average $650 million to $2.6 billion to launch a new prescription drug. And of course, not all drugs in development end up being approved. The investment in development, drug companies say, is why the prices have to be so high.
Rules for Medicare and Medicaid favor drug companies
In Medicare, all FDA approved drug types have to be made available, for the price set by the drug company. Medicare can’t negotiate lower prices—it’s actually against the law. Medicare has other special rules, too. Drugs that treat epilepsy, depression, cancer, psychosis and other mental conditions, HIV, or drugs that stop the body from rejecting a transplant, are called “protected classes.” While to goal of the protected class rule is to make sure people have a lot of options for treatment, it also means the drug companies don’t have much incentive to negotiate because the drugs have to be offered. In fact, drugs in protect classes get rebates of just 14 percent, even though they are usually the most expensive drugs.
Read “Searching for savings in Medicare drug price negotiations” for more detail.
In Medicaid, just like Medicare, every drug class must be covered. The difference is each state’s Medicaid agency can negotiate prices. In the end, the state must offer the drug, so the negotiation is around a company getting on the list of recommended drugs. Drugs not on the recommended list usually require preapproval.
What do experts say about the problem?
Most analysis ends up with the realization that high drug prices are result of federal laws that restrict competition along with laws that require Medicare and Medicaid to make all approved drugs available. Take a look at The High Cost of Prescription Drugs in the United States
Origins and Prospects for Reform from the Journal of the American Medical Association.
Why do prices keep going up?
Why do I keep paying more?
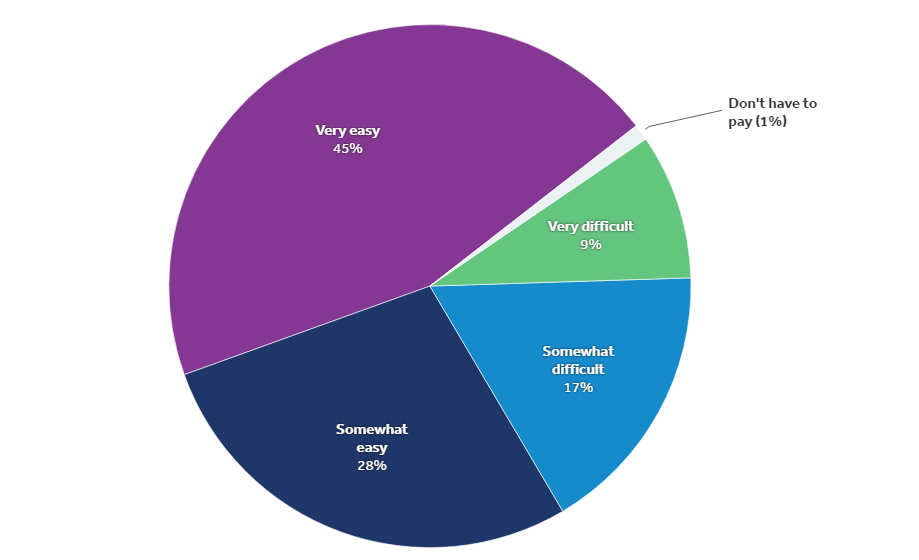
We pay for rising drug prices in two ways: in the premiums we pay each month, and though copays or coinsurance we pay when we pick up drugs at the pharmacy.
What we pay at the pharmacy depends on the drug we get. Most insurance divides drugs into levels. Tier 1 prescriptions are usually generic drugs that are the least expensive. Virtually all plans now have a specialty tier. Unlike copayments, coinsurance payments vary based on the list price of the medication. It’s common to pay about 25 to 30, sometimes even 40 percent of the price of the drug.
Drug prices are also figured into premiums. So even if you don’t take expensive prescriptions drugs, you are helping others pay for those drugs in the premiums you pay each month.
How much is spent advertising to doctors and potential patients?
U.S. is only one of two countries in the world that allow prescription drug advertising to citizens and physicians. Drug companies spend more than $6.4 billion a year advertising to patients and potential patients, and another $24 billion a year marketing to doctors.
Humira is the most advertised AND the best-selling prescription drug in the world. It started as treatment for Rheumatoid arthritis in 2012 for $1,500 a month. Now that same medication helps treat skin conditions, rigidity of the spine, an inflamed colon and more. Today, the price tag is $5,800 a month. This Chicago Tribune article from 2015 calls Humira the Swiss army knife of drugs and goes into detail about the company’s advertising and sales plans.
How is it possible that coupons increase prices?
You shouldn’t need a coupon to afford life-saving medications. Coupons wouldn’t be needed if the drug companies didn’t set list prices so high.
The federal government considers copay coupons to be an illegal kickback if used by someone who enrolled in Medicare or Medicaid. That’s because coupons encourage a patient to use a specific drug, with the rest of the expense picked up by taxpayers. It’s the same reason local health insurance companies have special rules in place for coupons.
Drug companies offer copay coupons for expensive brand name drugs. While a coupon can help one person afford medications for a while, unfortunately at the same time it allows drug companies to keep their prices high and pass those high prices on to everyone else.
The coupons effect how much we all pay for care especially when equally effective, less expensive options are available. Because drug companies don’t offer coupons to everyone who takes the drug nor do they offer coupons for the entire time someone needs a drug, everyone has to help pay.
What's the solution?
What's been tried & why hasn't it worked
Throughout the years, policymakers have tried to DO SOMETHING. But it’s hard to get at the root problem.
Examples of past attempts include when Congress decided to require a discount off specific kinds of drugs, or when it capped how much federal Medicaid will pay for a drug at a pharmacy. Drug companies comply, but can simply raise their list prices, making the discount ineffective.
How rebates save you money?
When insurance companies set prices for the premiums you pay each month, the rebates help lower that price. Regulators review that and other information to decide request is reasonable.
For people who get their health insurance through through corporations, the company decides how to use the rebate. According to Pharmacy Benefit Management Institute, employers they surveyed in 2017 did the following with the rebates:
- 68 percent used it to reduce what the company spent on prescription drugs
- 15 percent used it to reduce both what the company and the employees spend
- 11 percent reduced the premiums paid by employees
- 4 percent reduced what employees had to pay when they picked up drugs from their community pharmacy
- 1 percent responded that they did something else
What can help? Regulations.
Policymakers can make it easier to understand how drug companies set prices and where the money goes. While insurance companies have to get premiums reviewed and approved by regulators, and the companies have to report how they spend money each year, drug companies don’t have this kind of government oversight. Here’s a summary from America’s Health Insurance Plans about what some states are doing to help people understand rising drug prices.
What could help? Re-examine patent laws.
Patent laws are designed to protect intellectual property and allow drug companies to recoup investments. In some cases these rules are used to keep out competition, and this drives up drug prices.
Here’s more information from the FDA and the American Academy of Actuaries.
Forbes, Bloomberg Business Week and the American Pharmacist Association have articles about the topic.
What could help? Evaluate drugs independently.
When we have choices, we should have data on how effective one drug is compared to another. Some groups are starting to do this but we have a lot of work yet to be done.
In many instances the more expensive drug is no more effective than a less expensive alternative. In the U.S. we grant lifetime approval for drugs but do not independently evaluate the value of a new drug. And once a drug is evaluated based on how it worked for 300 to 3,000 people, it’s approved. Conducting independent evaluations and requiring FDA re-approvals would provide better information on how well the drugs work over time and in comparison to other options. This could help you understand if you really need the $1,000 toe fungus treatment or if the $5 option would work just as well.
What I can do?
Learn more about the drugs you see on TV before you ask for them at your clinic. Talk to your doctor about your options. Newer does not always equal better. Often newer drugs are a lot like medications already available and the minor differences, like a coating or how often you take the pill, could mean a big difference in price you pay.
Background and facts from AARP, CDC, Harvard, Kaiser, the Council and more…
More background
Fact sheets created by the Council
Data from the Association of Community Health Plans
Data from America’s Health Insurance Plans