
Through their work together at UCare, Dr. Julia Joseph-Di Caprio, Chief Medical Officer for UCare, and Pleasant Radford, Jr., Health Equity Officer for the health plan, are creating bridges that will bring about better care for diverse populations. The health plan is looking at everything from provider engagement to their internal functions to ensure health equity for members. The Council recently caught up with Julia and Pleasant to get their perspective on UCare’s health equity journey.
———
QUESTION: How long have you been with your organization and what’s been your journey to your role?
ANSWER: Julia – I’ve been with UCare since 2018 as SVP and chief medical officer. My health equity journey started even before I went to medical school in that I recognized early on that caring for people is connected to the way in which they live. Then as I went through medical school and began working at Hennepin County Medical Center, now known as Hennepin Healthcare, we knew that our work would only be successful if we address more than what was happening in the clinical context. It has only been more recently that I and many others have understood that structural racism (racist policies, procedures, systems) causes disparities in care and outcomes. Also, at UCare, we are fulfilling our role in addressing the social drivers of health and anti-racism within our work and with our provider partners.
Pleasant – I’ve been at UCare as the Health Equity Officer since 2020. I have always been fascinated at the fact that the United States spends a lot of money on health care, but our health outcomes are not much better than many other countries. My interest in health care began as a child because my mom was nurse, and so I got a chance to see her love for that work and the empathy she had for the patients she treated. My original plan was to be a medical doctor, but then I decided to take some time off before going to medical school to explore the world. Peace Corps was that opportunity. In that, I learned so much about public health. I realized in that small time that community plays a huge role in your health. I decided after that to focus more on the public health side instead of going to medical school. The jobs that I’ve had have really been a connective thread across that. Now, in my role at UCare as the Health Equity Officer, I’m leading this work to ensure that we are thinking of health and racial equity at a systemic level by working with and for communities to address their needs.

Q: Disparities in health care have always existed, but in your view, how have recent events – like the COVID-19 pandemic and the murder of George Floyd – impacted health equity work and where it is headed?
A: Pleasant – What we saw was greater cognitive dissonance between the idea of America and the reality of America. Many of us believe that America is the land of the free – that it is just, fair, and equitable. In fact, what we saw last year was the reality that America is not just, fair and equitable for everyone. I believe the murder of George Floyd served as the pinnacle where people realized: “I cannot believe that this is America.”
With COVID-19, people really saw the frailty of our health care infrastructure and how important public health is to improve the health of our communities. The pandemic allowed people more time to practice introspection and decide on what we need to change this. Both of these events – COVID-19 and George Floyd – impacted health equity because people now see how structural racism is a root cause. It is important for us to see the role that racism plays in healthcare, the role we play in enabling that system, and how we can start to change that system – the policies and procedures – to achieve health equity for all.
Julia – It wasn’t enough for people to say they were suffering from structural racism. People had to see someone murdered on camera before people would say “this is a thing.” I do believe the pandemic and its disproportionate effect on folks did advance the cause of addressing the structures that drive these impacts. I think the impact of the murder of George Floyd did accelerate things. I think our challenge now is to make this work even more sustainable over time. What I also reflect on is that, even for organizations like UCare that has years of partnerships with communities, some leaders are asking us about our commitment. We have to go with humility and recognize that many people have been advocating and doing this work for years, and we have to make sure that we take our direction from them. I also think we must honestly say that this is a curved path and there will be retrenching. I think we must recognize that even with all that happened over the last 15 months, we are not a point yet where this work is sustainable, and we need to build sustainability.
Q: What are some of the biggest barriers you see in delivering equitable care and what are steps that health plans can take remove those barriers and better connect with BIPOC communities?
A: Julia – I’ll speak to some of our core health plan work as it relates to ways in which we can remove barriers. For instance, with our work with providers, we will expect improvements in advancing health equity. I can see plans continuing to evolve and deepen that work including requirements around the diversity of the workforce in our partners. I could see core health care functions used to drive health equity.
Pleasant – Trust. I cannot emphasize that enough. There is a lack of trust in the health care system. That’s a huge barrier. If you are not able to trust the providers and the health care system to help in your journey toward optimal health, then it becomes difficult to stay healthy. Another part that I think is important to state is that health equity is a process and an outcome. We never completely “arrive” at health equity. We are constantly learning and re-learning. One barrier is that we often see it only as an outcome – we don’t respect the process that it takes to get there. You are going to make mistakes along the way. It is important to acknowledge those mistakes, say you’re sorry and continue to grow.
Q: What specific initiatives (committees, taskforces, work groups, cabinets, etc.) have been created at your organization to address health equity? And given these initiatives, what progress has been made in terms of making care more equitable?
A: Given the large number of members UCare serves who are most at risk of facing inequity, this work is embedded across many work groups, committees and subcommittees throughout UCare.
- UCare has a cross-department Health Equity Committee that identifies new opportunities, shares learnings and reviews updates on initiatives.
- Our Population Health team and subcommittees integrate health equity goals into all of their member health activities.
- Our Community Outreach teams contact members who face the most inequities to help them get their COVID-19 vaccines and connect them with community resources to avert social risk factors.
- Our Health Promotion Department has quite a few programs specifically directed to counter inequities especially around food insecurity.
- We are also kicking off an internal DEI work plan, which ties into health equity on all fronts. An Oversight Committee and Employee Advisory Committee helped drive and provide input for this plan.
Q: What role do you see partnerships (with the community, with the state, with others in the health care ecosystem, etc.) playing in advancing health equity efforts?
A: Pleasant – Partnerships are extremely important. It was one of the main reasons why I joined UCare. We have such a strong history of partnerships with the community. As I think about health equity, partnerships are the foundation of that. I believe partnerships help evolve and broaden our reach to strengthen our impact. As organizations, we see things through a certain lens, but it is not the only lens that will solve a problem or create a solution. Partnerships are key so that we leverage the unique assets and strengths we have to offer. They also allow us to contextualize health care and health equity within communities so that we better understand what is the right solution to reach optimal health. Partnerships teach us humility. We don’t know everything, so they allow us the learning and dialogue that must take place. Ultimately, our partnerships make us stronger in our work.
Julia – Some examples of partnerships include our work with the Minnesota Medical Association, funding their initiative to improve health equity, and Stratis Health, funding their work on their Culture Care Connection website. It is designed to help health care professionals by providing tools and resources to help them be responsive and supportive of the diverse patients they serve.
Q: What role does organizational culture and diverse staffing play in health equity? How can health plans use cultural competencies to improve health outcomes?
A. Pleasant – Organizational culture is so important. It undergirds how we operate, think and create policies, processes, and procedures for employees. As we think about health equity and culture, it’s important that our culture reflects the communities that we serve. We have to ensure that we have the right people in the right conversations to make the right decisions. When we make the wrong decisions, it costs time, money and lives. A diverse staff improves our work, our culture and the health of our employees and members.
Julia – The COVID vaccination development is a prime example of how quickly systems were able to adapt to the pandemic and provide care using significant technologies like ECMO and other things. That makes what happened last year so stark. You wonder if people brought the best thoughts to bear around the social drivers of health and advancing racial and health equity, would last year had been such a disgrace? Because that came from years of not addressing what we knew needed to be addressed. We need to bring the best minds to bear, which means diverse thinking, like we have for other health issues. If we brought that same thinking to bear in terms of advancing health equity, we would be able to solve it.
Q: Distrust in the health care system continues to be a huge challenge when it comes to health equity, which has been laid bare by lower COVID vaccination rates in communities of color, but impacts other care, also. How do we rebuild trust in BIPOC communities?
A: Pleasant – We have to combat a deficit-based mindset. If all you see are the stereotypes of an individual or community versus looking at them from an asset-based perspective – in the sense that they have a lot to offer and we can learn a lot from them – this will be a barrier. We have to ask ourselves: How can I be humble and engage in a dialogue with this person so we can offer equitable care? It will be important to take those steps so that we can continue to build that trust in our communities of color.

During her tenure at PreferredOne, Dr. Abbie Miller, the health plan’s Chief Medical Officer, has placed an acute focus on health equity. As a physician, she knows firsthand how critical it is to address health disparities in a meaningful way to improve patient outcomes. Asking the community for their preferences is a vital step. The Council recently caught up with Abbie to get her perspective on PreferredOne’s health equity journey.
———
QUESTION: How long have you been with your organization and what’s been your journey to your role?
ANSWER: I have been with PreferredOne for 2 years as the Chief Medical Officer (CMO). I am board certified in family medicine and I spent my career prior to PreferredOne in care delivery working as a hospitalist as well as medical director of care management and utilization management for a large system. In my role as a practicing physician, I came to the realization that there are problems inherent in the health care “system” that result in poor outcomes and health inequities that cannot be addressed simply through improving the doctor/patient relationship. This drove me to take on an administrative role so that I could help bring the lens of the provider to those larger “system” conversations.
Q: Disparities in health care have always existed, but in your view, how have recent events – like the COVID-19 pandemic and the murder of George Floyd – impacted health equity work and where it is headed?
A: I think that recent events have brought a new level of awareness and brought the conversation to the forefront. In health care, we have spent time examining the problem of health equity, often discussing “social determinants of health.” We recognize that health outcomes are different based on these factors, but my hope is this momentum will drive us to action rather than continued examination.
Q: What are some of the biggest barriers you see in delivering equitable care and what are steps that health plans can take to better connect with BIPOC communities?
A: I continue to see gaps in ensuring patients feel they can relate to their provider. This means we need more diversity in our provider networks, which starts with ensuring more diversity in our medical education programs. I think the best way to connect is to not presume we know what is desired or needed and instead have conversations with those in our community about their experiences and ask for input.
Q: What specific initiatives (committees, taskforces, work groups, cabinets, etc.) have been created at your organization to address health equity? And given these initiatives, what progress has been made in terms of making care more equitable?
A: At the health plan level, we are trying to gather more information about the providers and members covered by our plan. We want to know whether they are more comfortable speaking a language other than English, whether they are a person of color, whether they identify as LGBTQ. Then we want to make sure that our provider network is similarly diverse and that we not only identify a provider’s specialty but also what language(s) they speak and whether they are experienced in caring for LGBTQ persons. We are making slow progress on this given we have to overcome perception of the historical use of this information to discriminate.
As a system-owned health plan, our system owners have created the H.O.P.E Commission to better identify systemic issues that lead to disparities and create a plan to address those issues.
Q: What role do you see partnerships (with the community, with the state, with others in the health care ecosystem, etc.) playing in advancing health equity efforts?
A: I believe partnerships are crucial in this work as it will take a system-based approach to fix systemic problems. We must work together with community organizations to have hard conversations about shared past negative experiences, reach a common understanding about future needs and work together to create trust and a path forward.
Q: What role does organizational culture and diverse staffing play in health equity? How can health plans use cultural competencies to improve health outcomes?
A: As I stated above, we relate to one another through shared experience and shared history. Ensuring diversity throughout our health plan staff, just like our network, will help our diverse members feel more comfortable. It will also raise collective awareness and cultural intelligence across the organization.
Q: Distrust in the health care system continues to be a huge challenge when it comes to health equity, which has been laid bare by lower COVID vaccination rates in communities of color, but impacts other care, also. How do we rebuild trust in BIPOC communities?
A: We must work together with community organizations to have hard conversations about shared past negative experiences, reach a common understanding about future needs and work together to create trust and a path forward.

During his time at Hennepin Health, Michael Webber, the health plan’s Analytics and Health Economics Manager, has taken health equity initiatives head on. His work entails working directly with vulnerable communities to find solutions that will enable better health care. This involves intentional listening, learning — and doing. The Council recently caught up with Micheal to get this insights on Hennepin Health’s health equity journey.
———
QUESTION: How long have you been with your organization and what’s been your journey to your role?
ANSWER: I have worked for Hennepin Health for 3 years in analytics and health economics. I previously worked in accountable care organization (ACO) analytics at Fairview and in orthopedic bundled payments and lean at Avera Health in South Dakota. I came to Hennepin Health because I was excited to apply my skills at the intersection of finance, operations, and analytics at an organization with a mission to improve health care for members that often face social and behavioral health barriers. I believe analytics play a role in highlighting disparities and measuring the efforts to improve them.
Q: Disparities in health care have always existed, but in your view, how have recent events – like the COVID-19 pandemic and the murder of George Floyd – impacted health equity work and where it is headed?
A: I’m proud that Hennepin County and Hennepin Health were already prioritizing equity before the pandemic and the murder of George Floyd. These events brought attention to areas where we were already making investments.
Hennepin Health provided funding in 2019 for a Hennepin Healthcare project that improves prenatal care for American Indian and Black/African American communities through models of care that incorporate community-based and culturally responsive programming. The same year we provided funding for a pilot program at Northpoint called the Mama Mtoto program for Black/African-American mothers facing social barriers. We also have invested in recruiting and training doulas from groups that experience health disparities.
Q: What are some of the biggest barriers you see in delivering equitable care and what are steps that health plans can take to better connect with BIPOC communities?
A: In analytics, we are specifically focused on measuring disparities. We need to be able to measure disparities in order to know where to focus our efforts and to know whether or not our efforts are improving them.
At the same time, getting the perspectives of individuals in groups experiencing disparities is important. I previously mentioned a Hennepin Healthcare project that we funded. Hennepin Health conducted a series of ten listening sessions with 168 U.S. born Black/African-American and American Indian women that focused on the women’s current experiences with prenatal care, birth, and postpartum care as well as their suggestions for what would improve those experiences and increase engagement with care. Their input was invaluable in improving prenatal models of care for Black/African-American and American Indian women.
Q: What specific initiatives (committees, taskforces, work groups, cabinets, etc.) have been created at your organization to address health equity? And given these initiatives, what progress has been made in terms of making care more equitable?
A: Hennepin Health funded the Mama Mtoto pilot program at NorthPoint. Black/African-American women experience an infant mortality rate of 10.4 per 1,000 births compared to 5.1 per 1,000 births across all other racial groups in Minnesota. The program uses a psychotherapy support group structure to teach positive coping behaviors, self-regulation, and child management skills. The program simultaneously encourages prenatal and postnatal visits. Of the 43 women enrolled, 85% had prenatal care within the 1st trimester, 82% completed an obstetrics physical at time of enrollment, 100% had at least 6-8 prenatal appointments with their primary care provider, 100% have completed a postpartum visit, 100% had healthy birth outcomes, and 100% of the babies delivered have completed well-baby exams.
Q: What role do you see partnerships (with the community, with the state, with others in the health care ecosystem, etc.) playing in advancing health equity efforts?
A: Providers tend to have more direct relationships with our members so we tend to partner with our providers. We know to make a difference that we need to support and leverage patient relationships with providers. We can do more with our partners than we could ever accomplish otherwise.
Q: What role does organizational culture and diverse staffing play in health equity? How can health plans use cultural competencies to improve health outcomes?
A: Listening session participants from the Hennepin Healthcare project frequently mentioned the desire for doulas from the same cultural background as themselves. In response we provided funding for a program through the Cultural Wellness Center to recruit and train U.S. born Black/African American doulas. The goal is to establish a perinatal workforce across Hennepin Health’s provider network that reflects the diversity of the plan’s enrollees. The program trained 15 Black/African American doulas who are now registered with the state to provide doula care.
Q: Distrust in the health care system continues to be a huge challenge when it comes to health equity, which has been laid bare by lower COVID vaccination rates in communities of color, but impacts other care, also. How do we rebuild trust in BIPOC communities?
A: I believe listening is the key. I’m proud that a Hennepin Health-funded program led to listening sessions that solicited feedback from 168 people from BIPOC communities. We can point to specific funding for culturally specific doulas that arose from that effort. BIPOC communities are going to trust us more over time if we solicit their perspectives and implement concrete responses to what we hear. In the end, we believe people support what they help create.

Dr. Patrick Courneya, Chief Health Plan Medical Officer for HealthPartners, and his team are making major changes throughout the organization in an effort to address health disparities in Minnesota. This includes building an antiracist culture at HealthPartners and increasing the diversity of health plan leadership by 100%. HealthPartners has also engaged in conversations with members, patients and the community to better understand what they can do to build trust. The Council recently caught up with Dr. Courneya to get his thoughts on the health equity journey at HealthPartners.
———
QUESTION: How long have you been with your organization and what’s been your journey to your role?
ANSWER: I first joined HealthPartners in 1991 as a family practice clinician and later served as medical director and associate medical director for the health plan. In 2014, I joined Kaiser Permanente in Oakland, Calif., where I served as executive vice president and chief medical officer for national health plan and hospital quality. Following my six years at Kaiser, I returned to HealthPartners in January 2020 as chief health plan medical officer.
Q: Disparities in health care have always existed, but in your view, how have recent events – like the COVID-19 pandemic and the murder of George Floyd – impacted health equity work and where it is headed?
A: Across HealthPartners, we felt the upheaval of the dual pandemics of COVID-19 and racial injustice in our community. While this work isn’t new for us, the events of the last year put a sharper focus on the racism, injustice and health care disparities experienced by communities of color. In a very real sense, we are digging even deeper into the systemic drivers of inequity and assuring that we are actively changing ourselves and advocating externally to eliminate those drivers. HealthPartners has redoubled our commitment to improving health equity and effecting meaningful change for our members and patients of color – and we’re encouraged to see many organizations in our community doing the same. This is an ongoing effort, but we’re set up for improved accountability with our new goals, initiatives and partnerships.
Q: What are some of the biggest barriers you see in delivering equitable care and what are steps that health plans can take to better connect with BIPOC communities?
A: We know many people in communities of color and other underserved health populations face additional barriers to access the care they need. Today, HealthPartners has multiple approaches to removing these barriers for our members and patients and promoting accessible care for all. Some efforts include language services, transportation services and a mix of options for appointments, including telehealth, drive-up sites and other accessible care sites. We are also examining our coverage and other policies with an equity lens, working to assure they do not unintentionally interfere with achieving health equity. In addition, we have several initiatives and partnerships to address social determinants of health in our community, including building homes with Habitat for Humanity, providing respite care with Catholic Charities and improving access to healthy food with local food shelves. We’re always looking for opportunities to improve this work and build trust among those we serve.
Q: What specific initiatives (committees, taskforces, work groups, cabinets, etc.) have been created at your organization to address health equity? And given these initiatives, what progress has been made in terms of making care more equitable?
A: HealthPartners is accelerating our equity work by aligning existing efforts across the organization and taking a more intentional approach to address health equity. As part of our renewed focus on this important work, last year we formed the HealthPartners Equity, Inclusion and Anti-Racism Cabinet, made up of a diverse group of our organization’s leaders. Under the cabinet’s leadership, we’ve set ambitious, public goals to achieve by 2025, including:
- Increase the racial diversity of our leadership team by 100%
- Build an anti-racist culture and deepen our understanding of cultural humility
- Eliminate disparities in maternal and infant care
- Eliminate disparities in childhood immunizations
- Eliminate disparities in chronic conditions and preventive screenings
Q: What role do you see partnerships (with the community, with the state, with others in the health care ecosystem, etc.) playing in advancing health equity efforts?
A: HealthPartners has always had a strong sense of health care partnership in our community. Health – for all people – is a team sport, and our communities are stronger when we can pull organizations together to build momentum, push for change and achieve common goals. As part of the HealthPartners 2025 Partners for Better Health Goals, one of our primary areas of focus relates to building partnerships in the community, because we know much of what contributes to an individual’s health and well-being happens outside of the health care system. In addition, we’re committed to building upon our current community partnerships with health equity at the forefront, including Make It OK, Little Moments Count and PowerUp.
Q: What role does organizational culture and diverse staffing play in health equity? How can health plans use cultural competencies to improve health outcomes?
A: Building a culture of inclusion in the workplace is critical for HealthPartners to provide quality care and health equity for every patient and member. We’re committed to being an organization where every person is welcome, included and valued – because when we embrace diversity, we’re better positioned to provide quality care to our members, patients and communities. Initiatives like our community health worker program prioritize connecting members and patients to those who share culture-specific knowledge, skills and values so more people feel represented, comfortable and empowered in their health care decision making.
Q: Distrust in the health care system continues to be a huge challenge when it comes to health equity, which has been laid bare by lower COVID vaccination rates in communities of color, but impacts other care, also. How do we rebuild trust in BIPOC communities?
A: The pandemic cast new light on the ongoing issue of health disparities in our community. COVID-19 disproportionately affected communities of color, and we recognize the issues of mistrust in our community and the health care system. Some of the work HealthPartners is currently doing to build trust among our members and patients involves learning about their unique experiences within the health care system. We’ve engaged in conversations with our members, patients and community to better understand what we can do to build trust, address bias and provide a more welcoming environment for people of all backgrounds. Through these important conversations, we’ve gained new perspectives on how to better care for and serve people and have implemented changes based on what we’ve learned. This is an area of focus for us, and we’ll continue to work closely with all those we serve in order to build trust and ultimately improve health outcomes.

Minnesota’s nonprofit health plans are placing a renewed focus on health equity, recognizing how pervasive health disparities are in our state. Health plans are looking at everything from workforce diversity and training to ways in which they can better deliver care and access to communities of color. Over the next few weeks, the Council will be highlighting their efforts through Q&A interviews with health plan leaders. We start with Cara Broich, Medica’s Senior Director of Quality and Clinical Advancement.
———
QUESTION: How long have you been with your organization and what’s been your journey to your role?
ANSWER: I have been with Medica for 29 years. Prior to working for Medica, I was a Cardiovascular ICU nurse. Throughout my tenure at Medica, I have worked in various roles focused on quality and population health. My role in health equity came naturally out of my interest to improve the health of our members and communities. I lead the Health Equity Workgroup and Health Equity Leadership Subgroup at Medica.
Q: Disparities in health care have always existed, but in your view, how have recent events – like the COVID-19 pandemic and the murder of George Floyd – impacted health equity work and where it is headed?
A: Although health inequities have always existed, the COVID-19 pandemic and the murder of George Floyd took our focus on these inequities to another level. Now it is much easier to get the support needed to move initiatives forward. On one hand, it is disheartening to realize that it took a video recording of a man’s murder, and a pandemic, to really enable us to gain traction on these initiatives.The level that our initiatives have been elevated to, and the support we have received from across the organization, and our board, has been overwhelming. I am excited to see how our work will address health inequities in our community.
Q: What are some of the biggest barriers you see in delivering equitable care and what are steps that health plans can take to better connect with BIPOC communities?
A: There are multiple issues that hinder the delivery of equitable care. One of the biggest is that the medical community hasn’t focused on it. Historically, most medical studies were conducted on white males and medical guidelines were developed around those studies. We need to take a step back and look at guidelines and policies with an equitable lens. When we find that a guideline, policy, or practice has directly or indirectly contributed to the development of a barrier, we must take action and make changes. Where changes are made, our BIPOC community leaders will need to be informed about how the changes may have a positive impact on our diverse citizens. We must show that we are taking action in order to gain the trust of members of communities who have been marginalized for generations.
Another barrier is the availability of data. We do have race, ethnicity and language data for our Medicaid population, however for the Commercial, Medicare and individual business, data is extremely limited. This forces us to use generalized data from other sources. To truly be able to improve care, we need to be able to measure what is going on within a population and then work in partnership with the BIPOC community to address the issues. Connecting with community organizations is truly the key to improving care. Medica has hired staff to focus on community partnership, but again, the data is lacking for non-Medicaid populations. I can use data to identify the issues, but it is critical to work with the BIPOC community to develop ideas on how to address the issues. Only in partnership can we improve health inequities.
Q: What specific initiatives (committees, taskforces, workgroups, cabinets, etc.) have been created at your organization to address health equity? And given these initiatives, what progress has been made in terms of making care more equitable?
A: Medica formed a Health Equity Workgroup in June of 2020. The workgroup is focused on Medica’s Health Equity mission to assist our members in attaining their highest health potentials. We are committed to health equity, which holds that no person be disadvantaged from achieving their potential, as a result of barriers. We consider the many characteristics that make people unique – such as race, ethnicity, gender, sexual orientation, abilities, age, socioeconomic status, or veteran status – because any of these differences may be the basis for disparities in health care access, experience and outcomes. The workgroup is made up of people from across, and at all levels, of the company. The principles and commitments that guide our health equity work align with four areas of focus; they include:
- Leadership and decision-making
We will seek diversity in our representation and engagement to guide our work and decision-making at all levels of Medica, including our work group and leadership activities, and in our decision-making, policy and program development.
- Data practices
We will expand our data collection efforts, where appropriate, to guide necessary health equity interventions and evaluate our health disparities reduction efforts.
- Policies and procedures
We will examine our policies using an equity lens and make policy changes needed to promote equity, reduce health disparities, and eliminate barriers or unintended impacts on historically underrepresented and/or marginalized groups.
- Access and outcomes
We will review and develop policies and care models that improve access to care and community resources that meet our members’ diverse health-related social needs and preferences.
We decided to start by taking a tactical approach to health equity and have addressed many small areas first:
- Volunteered our staff to the Minnesota Department of Health to complete contact-tracing phone calls during the height of the pandemic.
- Reached out to our membership groups that were most affected by the pandemic to ensure they had their needs met and provided resources if necessary.
- Expanded the scope of our Network Access and Availability committee to ensure Medica offers sufficient, equitable and culturally competent provider access and availability across the member demographic groups it serves.
- Expanded the Quality Improvement and Care & Utilization Management committees to include a focus on health equity.
- Added specific health equity goals to both the Quality Improvement and Care & Utilization Management 2021 work plans.
- Developed a health equity rubric to evaluate Medica’s policies and procedures to ensure they are not hindering health equity. As policies come up for review, we are using the new tool to conduct the evaluation.
- Conducted a deep dive into the diagnosis of hypertension to test new data related to social determinants of health, race, ethnicity and language. This enables us to not only focus on a common disease state, but also test out new data sources. We are in the process of developing interventions based on our findings as well as expanding our data collection sources.
- Modified the criteria used in Medica Foundation grant process to further expand the evaluation of proposals based on their impact to health equity.
- We are partnering with a clinic that serves mostly underserved populations to assist them in their COVID-19 vaccine efforts by providing volunteers.
- Following the murder of George Floyd, we reached out to our members who lived in affected communities to assist them in obtaining health care and prescriptions.
- Reached out to our Medicaid enrollees to assist them with scheduling COVID-19 vaccinations and arrange for transportation.
Q: What role do you see partnerships (with the community, with the state, with others in the health care ecosystem, etc.) playing in advancing health equity efforts?
A: No one organization can solve the problems, however, if we work in partnership we will be able to work toward a solution together. These are very complex issues that involve all aspects of health care; from the way medicine is practiced to social determinants of health to trust issues. Through partnership with the State, health plans, providers and community organizations, we will make progress.
Q: What role does organizational culture and diverse staffing play in health equity? How can health plans use cultural competencies to improve health outcomes?
A: Organizational culture and diverse staffing play a very important role in health equity. It brings forward diversity of ideas and opinions that lead to better, more equitable decisions. In an effort to reduce health disparities, you must truly understand the diverse communities that are impacted. The best approach to understanding these communities is to immerse yourself in their culture and allow that culture to weave itself into the fabric of the company’s practices, policies and behaviors. Employee cultural competency plays a critical role in improving health equity. It allows staff to understand where various members are coming from and what needs they may have. It allows for empathy. It also emphasizes that diversity of experience and ideas is a good thing, which leads to creative problem solving.
Q: Distrust in the health care system continues to be a huge challenge when it comes to health equity, which has been laid bare by lower COVID vaccination rates in communities of color, but impacts other care, also. How do we rebuild trust in BIPOC communities?
A: Truly partnering with the BIPOC community is critical. We need to work with the trusted organizations within each of the communities to improve health equity. This needs to be a true partnership – not the health care system telling them how to solve the problems but really listening to their needs and working together to solve the issues. We must acknowledge how the mistrust has developed, own our contributions to its evolution, and take strides to gain the trust that we will need to be successful. We all must realize that this trust must be earned and may not be easily obtained. We must commit to taking action based on what we hear from our BIPOC communities.
When the Council asked health plan employees why they chose to receive the COVID-19 vaccine, one thing was abundantly clear: They wanted to do their part to protect the community. We are sharing their stories of what motivated them to get vaccinated — and why they are also encouraging others to do so.
“I took one for my Hmong community to show them that the vaccine is safe and effective. And it is not only about protecting my family and myself, but the community as a whole,” said Pang Cha, Community Relations Supervisor, UCare.

“I got vaccinated to protect myself and my family. I wanted to protect my Native community and elders. Indigenous populations experience more severe outcomes and higher rates of death from COVID-19, and we need to do everything we can to protect our culture, including our people who have the knowledge that we depend on,” said Quanah Walker, Director of Behavioral Health Services, HealthPartners.

“COVID is the real enemy. Getting the vaccination helps me not to get it. I got the vaccination so that I can feel safe and do my part to make everyone safer,” said Jill Lantto, Complex Case Manager, Medicare Advantage, BCBS Minnesota.

“I’m looking forward to getting back to traveling abroad,” said Cara Broich, Senior Director, Quality & Clinical Advancement, Medica.

“I have to admit I was hesitant at first about receiving the COVID vaccination. But I am 58 years old and have asthma, and COVID could be very dangerous for me. So I made the choice to get the vaccine,” Lori Osberg, Claims Examiner, PreferredOne.

“Getting my second dose was important to boost my protection and stop the spread,” said Lucas Nesse, CEO, Minnesota Council of Health Plans.

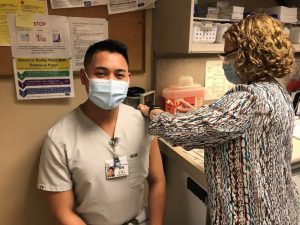
“My work as a nurse is rooted in science and empathy. Getting vaccinated is backed up by evidenced-based research. I am eager to help my community, especially those who are high risk, work the front lines and part of marginalized groups,” said Justin Juan, RN, Methodist Hospital (HealthPartners).
“I was a little hesitant to get the vaccine at first, but I decided to get it because I felt that the benefits outweighed the risks and I want to protect myself and others. I am super COVID leery, and I want to be able to travel and visit family and friends without fear of getting myself or someone sick,” said Carla Foster, Individual & Family Sales Specialist, UCare.

“I’m looking forward to getting back to hikes with my mom,” said Keely Brenno, Director of Communications, Medica.

“I believe in the science behind the vaccine. I believe that is the quickest way back to normalcy. Back to enjoying all those things we love, without putting the people we love at risk,” said Debby Erickson, Medicare Sales Specialist, UCare.

“I want to be protected from COVID-19 and I want to do everything I can to keep others from getting COVID-19,” said Dr. Julia Joseph-Di Caprio, Chief Medical Officer, UCare.

“I wanted to be protected from COVID-19 myself and to do my part to keep others from getting COVID-19 from me. I knew I was protecting my children, grandchildren, friends and anyone I come in contact with,” Ghita Worcester, SVP and Chief Marketing Officer, UCare.

“I did so because I am doing my part! For the health of my family, friends, neighbors — the whole community,” said Patty Butenschoen, Provider Database Specialist, PreferredOne.

“It’s time to put an end to all the death and heartache. I want to be part of the solution in protecting our community from this awful disease,” said Jocelyn Parker, Director of Communications, Minnesota Council of Health Plans.

“What would be the point of all the pain, abuse, and sacrifice that my African-American ancestors endured if I wasn’t willing to stand up and keep fighting? This question played in my mind as I rolled up my sleeve to get the vaccine. My community has endured a lot. We have gotten this far on our journey towards better health – why stop now? Let’s commemorate the sacrifices our ancestors made and protect ourselves so that we can continue the fight to build a better health care system that reflects us and partners with us on our health and well-being,” said Pleasant Radford, Jr., Health Equity Officer, UCare.

To find a vaccine location near you, visit the State of Minnesota’s Find My Vaccine tool.
From helping vaccinate our health care heroes to hitting the road in modified city buses to reach underserved communities, Minnesota’s nonprofit health plans are rolling out creative strategies to fight the COVID-19 outbreak.
This work starts with the equitable distribution of the COVID vaccine and increasing vaccine confidence. Health plans are stepping up efforts to make access to immunizations easier for vulnerable communities while also providing vital information to those who are vaccine-hesitant or have questions about the vaccine. Health plan employees are also sharing their own stories of why they chose to get vaccinated to encourage others to do so. These efforts are especially important as statistics show that COVID vaccination rates in communities of color are lower than those of whites even though mortality in some populations of color can be significantly higher.
Partnering to immunize for impact
A key initiative under way is a collaboration between the Minnesota Council of Health Plans, the Minnesota Department of Health, the Minnesota Department of Human Services, and the Minnesota Association of County Health Plans to immunize for impact by tailoring vaccine outreach and distribution to health plan members in ZIP codes with high Social Vulnerability Index scores (SVI).
The SVI takes into consideration 15 social factors, including poverty, disability status, lack of transportation access, and housing status, to identify areas most in need of vaccine services. While 31% of all Minnesotans live in a high SVI ZIP code, it is much higher when stratified by race, with 57% of American Indians and 55% of Black Minnesotans living in a high SVI ZIP code. High SVI ZIP codes are almost evenly split between the Twin Cities Metro and Greater Minnesota, meaning this partnership will reach Minnesotans across the state.
The health plans will work with the state to contact members and provide information on vaccination, assist with scheduling appointments and help plan for their vaccination, including arranging transportation or other services, if needed. Data collected from this partnership will also help inform future public health outreach efforts, including COVID vaccination campaigns for kids.
Getting things rolling
Blue Cross and Blue Shield of Minnesota (BCBSMN) has climbed aboard a program with agencies including MNDOT and Metro Transit to deploy mobile vaccination units. The program uses Metro Transit buses that have been temporarily converted to rolling vaccine clinics. These mobile clinics serve people of color; urban Native Americans; LGBTQI+; people with disabilities and unique health needs; and people experiencing homelessness. Meanwhile, a group of registered nurses from BCBSMN teamed up with North Memorial Health to hold a vaccine clinic in Brooklyn Center. The nurses not only put shots in arms, but also took up the arduous task of prepping doses. “I feel passionate about vaccinating people because it will save lives,” said Jill Lantto, an RN with BCBSMN who volunteers at N. Memorial to give COVID vaccinations.

Outreach and teach
UCare and trusted community leaders are working together to build public confidence in the vaccine among people of color and other at-risk Minnesotans. The health plan’s COVID-19 vaccine outreach includes sponsoring clinics in the Cedar Riverside Somali community and educational videos in English, Hmong, Spanish and Somali featuring voices of respected community leaders. UCare is also holding drive-thru vaccine clinics for members at its headquarters in Northeast Minneapolis. Volunteers from UCare helped vaccinate health care workers and school employees, as well.
Show up, drive up and measure up
HealthPartners is making vaccine equity a top priority. Vaccine clinics are being intentionally held in diverse communities. For convenience, in-person and drive-up appointments are available – some on the weekends. HealthPartners doctors are also reaching out through social media, news media and directly to patients. The organization is tracking the results of this work to uncover new opportunities to make a difference.
Supporting the front line
PreferredOne volunteers stepped up early to help short-staffed clinics vaccinate critically important front-line health care workers, helping them be healthy enough to provide care to communities at higher risk. Said one volunteer: “After months of caring for patients with COVID, it was so rewarding to see our front-line staff smile with a sense of relief that their vaccine returned a sense of hope for themselves and for all of us.”
Meet those who lead by example
Over the next several weeks, the Council will be featuring health plan employees on our social media platforms who will share their reasons for getting vaccinated against COVID-19 and why they feel it’s critical to be an example for others. Their stories are both heartfelt and personal. We also believe they are inspirational and will help convince more people to get vaccinated.
“I got vaccinated to protect myself and my family. I wanted to protect my Native community and elders,” said Quanah Walker, Director of Behavioral Health Services at HealthPartners. “Indigenous populations experience more severe outcomes and higher rates of death from COVID-19, and we need to do everything we can to protect our culture, including our people who have the knowledge that we depend on.”
“My community has endured a lot. We have gotten this far on our journey towards better life and better health – why stop now?” said Pleasant Radford, Jr., Health Equity Officer for UCare.


Minnesota’s insurance companies support all Minnesotans by protecting the lives, property and well-being of families and businesses.They also bolster the state’s economy by providing tens of thousands of jobs and investing billions in the community.
For health plans, this includes investing in innovative models of care; working with community organizations and stakeholders to make social and environmental conditions healthier for members; providing wraparound services that support members in taking their medications, getting to their appointments on time and coping with emotional stresses; and supporting the broader economy through workforce growth and robust community giving.
In this video featured at the recent Insurance Day at the Capitol, Lucas Nesse, CEO of the Minnesota Council of Health Plans, joined the leaders of the Insurance Federation of Minnesota and the Minnesota Insurance and Financial Services Council to discuss how insurers are with Minnesotans throughout their journey.

This month, Nicquel Terry Ellis of CNN moderated an outstanding group of expert panelists and guests who participated in a discussion on ways to promote health equity through Medicaid contracting in Minnesota.
The virtual event was hosted by the Minnesota Council of Health Plans and the University of Minnesota’s Division of Health Policy and Management. The discussion centered on ways to build trust and innovation in our health care system to allow everyone a fair chance at good health. The Council appreciates the insights of Dr. Julia Joseph-Di Caprio of UCare, Dr. Nathan Chomilo of DHS and others who are advancing health equity efforts in our state.
You can hear a replay of the virtual event here.

At a time when COVID-19 is hitting communities especially hard, nonprofits — now more than ever — are playing a critical role in ensuring health and well-being. Whether you are in health care, human services, education, the arts or another sector, it’s important to talk about your nonprofit mission and what you are doing to help others. Why? Because the more people know about what you do, the more your services can reach the folks who need them most.
In health care specifically, operating a nonprofit health plan means being accountable to people, not just numbers. During the COVID-19 pandemic, nonprofit health plans worked across sectors to meet the needs of Minnesotans – supporting local food banks, investing in education programs and addressing the equity of care in our state. Health plans have also stepped up to waive cost-sharing for COVID-19 testing and treatment.
Read more about how nonprofits support the community in this article Minneapolis-St. Paul Business Journal.